Thanks for visiting the official website and blog of the University Health Network and Mount Sinai Hospital Osteoporosis Program.
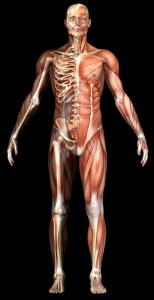
Osteoporosis is a major public health concern, with over 2 million Canadians currently suffering from the disease. This figure is expected to rise to 6.9 million by the end of the year.
Our clinic, led by Dr. Angela M. Cheung, provides diagnostic and clinical services to osteoporosis patients and people with low bone mass (referral). Every year, over 3000 patients walk through our clinic doors! We also have a dynamic research programme that is led by expert physicians and researchers in the field.
Please feel free to browse our website to learn more about osteoporosis, the research we conduct, and important tips for better bone health!
Participants Needed for osteogenesis imperfecta study